TO SCHEDULE AN APPOINTMENT CALL (703) 352-3520
CORNEA AND PUPIL
Michael O. Hughes, M.S.
Department of Ophthalmology
University of Virginia, Charlottesville, VA
Craig A. Luce, MSMI
Atlanta, GA and
Charlottesville, VA
Knowledge of human eye anatomy is important to medical illustrators and ocularists. Medical illustrators are professional artists with extensive training in medicine and science who render anatomy for educational purposes. Ocularists are trained technicians skilled in the arts of fitting, shaping, and painting ocular prostheses; matching patients’ fellow (living) eyes as precisely as possible. These professions sometimes overlap, with medical illustrators becoming ocularists. Members of both professions strive to depict anterior eye anatomy with artistry and accuracy. The purpose of this paper is to describe artistic techniques of vital interest to artists engaged in depicting eye anatomy, both two and three dimensionally.
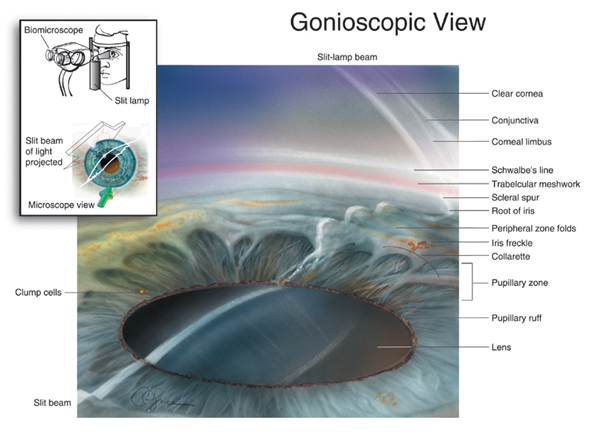
Figure 1
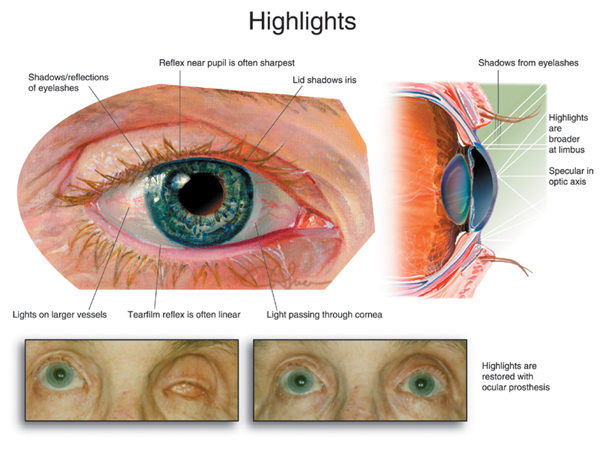
Figure 2
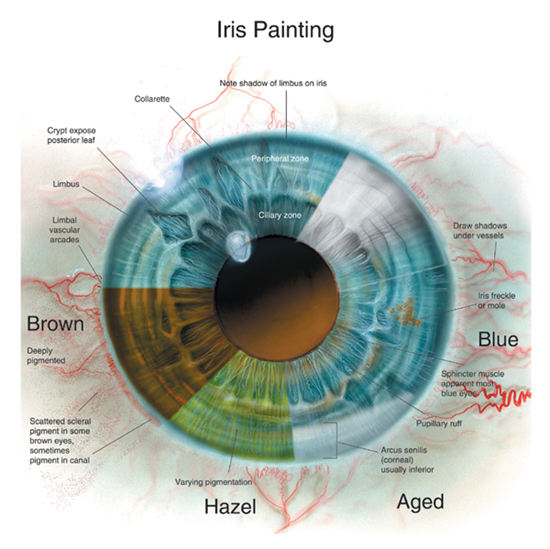
Figure 3
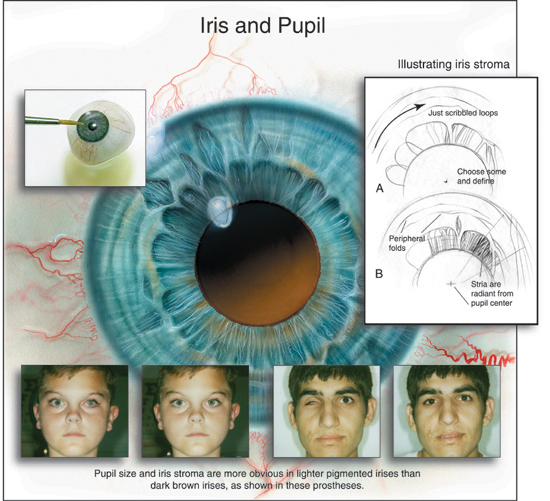
Figure 4
The visible portion of the human eye is of universal interest. This so-called “window to the soul,” figures prominently in many disciplines, from portraiture to mystical interpretation (iridology) to personal identification via computer analysis (biometrics) (Daugman, 1998). Medical illustrators and ocularists have a particular interest in accurately depicting the anterior anatomy of the eye. Medical illustrators help educate physicians and patients with depictions of anatomy that appear in articles, textbooks, and other materials. Ocularists fit and fabricate prosthetic (“artificial”) eyes.
Whether for cosmesis or educational purposes, the creation of aesthetic and accurate depictions of eye anatomy is a goal both ocularists and illustrators share. Materials, methodology and technology challenge both professions. However, with certain exceptions, they share a common approach: the ocularist “paints” in three dimensions and the medical illustrator in two dimensions. Professionally, the fields sometimes overlap, with medical illustrators becoming ocularists.* While many medical illustrators take courses in human anatomy and ophthalmological illustration, this article will present information sometimes forgotten or overlooked in depicting anterior eye anatomy in two and three dimensions. Therefore, it is the purpose of this article to describe techniques for depicting anterior eye anatomy in two and three dimensions. Part I of this article deals with the cornea, pupil, and iris. All eyes depicted in illustrations are the right eye (oculus dexter or OD).
THE CORNEA
While this transparent ocular structure is essential to visual function, the importance of creating a realistic cornea in prostheses and in illustrations is often overlooked. Medical textbooks offer several formulas for drawing the cornea but, as others have noted, these mainly emphasize the different radii of the anterior and posterior surfaces (Warren, 1988). Ocularists and illustrators specializing in ophthalmology recognize that the corneal shape is the structure most important in portraying reflected light. The corneal curve is best observed in cross-sectional illustrations. If the illustration fails to show the varying thickness of the cornea from center to margin, the illustrator has not accurately depicted the author’s written explanation.
Many ocularists make the cornea a perfect partial sphere. While this practice is acceptable, it should be noted that the cornea is spherical only at the central optical axis. From this central portion (3-6 mm in diameter, 0.3-0.5 mm thick) to the periphery (0.8-1.0 mm thick), the curve of the cornea flattens out. Reflections appearing near the limbus, the area where the transparent cornea joins the white scleral surface of the eye, are wider and less regular than those at the cornea’s center. For both ocularist and illustrator, reproducing these anatomical subtleties creates a more natural and accurate appearance
For illustrators, the best way to show the more diffuse highlights on this flatter portion of the eye is to create a semi-lucent shape that fades in opacity and lightness from the source to the reflected surroundings (Figure 1).
The shape of the cornea is revealed by reflections, also called reflexes, highlights, wet-lights, or catch-lights. In the living eye, the highlights fall in the same place on both corneas, signaling to the viewer that the eyes are looking in the same direction. If they did not, the gaze would appear to either diverge or converge, giving an undesirable “wall-eyed” or cross-eyed appearance. In both life and art, highlights at the eyelid margin reveal whether the eye is wet or dry. In ocularistry or illustration, therefore, few or no highlights suggest a dry eye; extensive highlights portray an eye brimming with tears.
Highlights appear naturally on the surface of a lubricated artificial eye. Regular buffing of the surface of an ocular prosthesis, coupled with teaching patients how to keep it lubricated, can prevent the artificial eye from appearing dull. The highlight of an artificial eye may appear asymmetrical with the contralateral or fellow eye for several reasons. For example, the prosthesis may not fit properly; as a result, the primary gaze of the prosthesis does not match the primary gaze of the fellow eye. Or, the prosthesis may have less motility than its fellow eye, thus lagging behind. Just as an inadequately highlighted prosthesis can suggest a dry eye, a prosthesis that is too dry will appear unnatural because it lacks the highlights present in the fellow eye. The ocularist may apply mineral oil or a silicone-based product to help the prosthesis move more comfortably and reflect light more realistically.
In medical illustration, highlights can be used as visual markers to direct the viewer’s attention away from the eye itself to surrounding details, as in illustrations of lid or facial surgery. Drawing or painting highlights that overlap the pupil, limbus, or both will visually break up these structures into partial circles, softening the effect of a direct gaze. The light in such illustrations appears to be reflected from something just in front of the iris (Figure 2).
The illustrator painting a reflection should take note of the natural anatomical barriers to reflection, such as the nonreflective eyelid and lashes. Including the nonreflective area in the limbal area of the highlight, just beyond the cornea, helps establish the eye’s position in space as well as the lid’s apparent position. Depicting highlights as not perfectly regular but as interrupted by natural anatomical features is a fine point that many illustrators, including portraitists, miss.
Medical illustrators add highlights to give the illusion of three-dimensionality to a two-dimensional illustration. In depicting a transparent curved surface such as the cornea, the illustrator will softly darken the area around the highlight to make it stand out. This can be done in PhotoShop by lassoing the intended reflection, making it wider towards the limbus than at the center, and then omitting the edge, which may be a shadow from the lid. The highlight will be curved to reflect the shape of the lids above it, and filled with a white gradient (foreground to transparent). This technique also can highlight the transparency of the cornea against the texture of the iris and conjunctival vessels. In summary, to achieve a realistic anatomical depiction of the cornea, one must accurately represent reflections off the cornea’s transparent surface.
THE PUPIL
For the purposes of illustration, the pupil is a circular orifice in the center of the iris through which light rays enter the eye. Anatomically, the pupil is located precisely in the iris’ center. To the viewer it appears to be positioned slightly above center and towards the nose. As a general rule, the diameter of the pupil is approximately one-third the diameter of the iris, ranging from 2-4 mm. The size varies depending on the sphincter and dilator muscles controlling pupillary contraction and dilation. In depicting surgical procedures the illustrator may, for accuracy, show the pupil as dilated or contracted: contracted during glaucoma treatment (e.g., iridotomy), dilated during cataract and vitreous surgery. In illustrating procedures conducted in darkened rooms, it is also worth noting that most of the active ciliary area inside the iris collarette will seem to disappear as the pupil enlarges to admit more light.
Illustrators use a compass (or circle marquee in PhotoShop) to form a perfectly round pupil. Both illustrators and ocularists blend accuracy and artistry, shading the pupil to enhance realism. While some ophthalmologists may complain that a pupil too altered or lightened from the black looks like a cataract, minimizing the compositional power of the plain, dark circle is important. A bit of blue in the dark pupil makes it appear to recede and creates an impression of three-dimensionality; a graded orange suggests the retinal reflex. The natural pupil appears black because it does not allow light back out, but artful gradation softens the circle in illustration (Figures 3 and 4).
Ocularists create the pupil mechanically by attaching “buttons” or “blanks” to the prosthesis. The button representing the pupil can be ground to match the pupillary diameter of the fellow eye. In addition, the ocularist may use a flat gray or brown plastic disk to represent both pupil and iris. This technique also is used when fabricating the thin, curved scleral cover shells worn over eyes that have lost vision but that remain in their sockets. Another technique requires the ocularist to simply center a pupil of thin emulsion or vinyl on the base of the iris button (Erph, 1946).
The authors, representing the fields of ocularistry and medical illustration, want to share their knowledge of anatomy and technical tips they believe are of vital interest and importance to both professions. Members of both professions and others engaged in depicting the human eye can achieve excellent results by combining knowledge of anatomy, experience, observation, and technical skills to duplicate the subtle anatomical variations in the cornea, pupil, and other living structures. Those variations can mean the difference between attaining, pictorically, anatomic accuracy; prosthetically, they yield an attractive appearance or unacceptable results.
Acknowledgements
For their critiques, review and encouragement, the authors thank Howard Bartner, Chief of Medical Illustration (Ret.) at the National Institutes of Health, Bethesda, Md; Ranice W. Crosby, Associate Professor of Art as Applied to Medicine, Johns Hopkins University School of Medicine, Baltimore, Md; Sara A. Kaltreider, M.D., of the Department of Ophthalmology, University of Virginia, Charlottesville, Va; and ocularist Joseph LeGrand of LeGrand Associates in Philadelphia, Pa. They also wish to thank Victor Weaver (www.victorweaver.com) for graphic design and Genevieve J. Long, Ph.D., of Portland, Ore., for writing and editing assistance.
References
Daugman, J. 1998. Phenotypic versus genotypic approaches to face recognition. In Face Recognition: From Theory to Applications. Heidelberg: Springer-Verlag.
Erpf, S.F., Wirtz, M.S., and V.H. Dietz. 1946. Plastic artificial eye program, U.S. Army. American Journal of Ophthalmology 29 (8):984.
Warren, L.A. 1988. Basic anatomy of the eye for artists. The Journal of Biocommunication 15 (1):22-31.
Authors
Michael O. Hughes is an ocularist who has been in private practice for more than twenty years in suburban Washington, D.C. (Vienna, Virginia). He is also the primary ocularist for the Department of Ophthalmology, University of Virginia, Charlottesville, Virginia. His website can be found at www.artificialeyeclinic.com. Craig A. Luce is a medical illustrator working in Atlanta and Charlottesville, Virginia. He has painted ophthalmic anatomy and surgery for 28 years. Among his work are 75 images for The Ciba Collection of Medical Illustrations, Vol. 8, Part III. Samples and CV are at www.medical-illustration.com. The authors have collaborated on many projects at the University of Virginia, including revisions to A Singular View: The Art of Seeing With One Eye by the late Frank Brady.
© 2005, The Journal of Biocommunication, All Rights Reserved